When running a medical practice, providing top-level care to your patients is of the utmost importance. Unfortunately, the complexities of medical billing and the claims process provide the opportunity to avoid medical billing fraud, abuses & errors.
Without regular financial oversight, certain individuals can suck the hard-earned money out of your business. It can also put you at risk of claims rejection by insurance and cause compliance issues.
Fortunately, by understanding the ways by which certain actors can take advantage of your practice, and how to identify them and place safeguards in your billing infrastructure, it is possible to greatly reduce medical billing fraud, abuses, and errors.
Understanding healthcare frauds & abuse
In the health care industry, fraud and abuse are used to describe different types of reimbursement problems. Here are some examples of healthcare fraud and abuse. ninja download manager pro license key
Fraud by Patients and Identity Thieves
- Insurance Scams – Scammers often utilize emails and telephone numbers in order to convince them to enroll in phony health care plans, bill them for non-rendered services or steal their identities.
- Falsifying Insurance Information–A patient who provides fraudulent insurance information in order to receive free or subsidized care.
- Receiving a Prescription with Intent to Sell–patients can commit fraud by faking symptoms or by exaggerating the severity of those symptoms to receive more medication to sell for a profit.
Fraud By Medical Providers and Practitioners
Practitioner fraud occurs when a doctor, nurse, administrator, or others use the power of their situation to defraud their employer, their patients, or an insurance company by way of medical billing company. One common way this type of fraud occurs is when a practitioner bills for a medical service that is unneeded in order to gain a profit. A patient can also be billed twice for the same procedure. Sometimes, visits can be fabricated entirely. This type of fraud can bring your business a lot of negative attention and legal problems if it isn’t identified right away. sketchup pro /a>

How to Prevent Errors in the Medical Billing Process
Information mismatch happens in medical billing process. The first step in preventing errors in your medical billing is to ensure that any personal information (such as age, name, race, gender, and policy information) of your clients is accurate.
Healthcare errors and even fraud can be further prevented, by regularly auditing your billing claims. This means making sure that: the itemization is clear; the coding is free from errors and is up to date and the reimbursement amount is correct and reflects the services rendered.
Ways to Avoid Medical Billing Fraud & Abuses
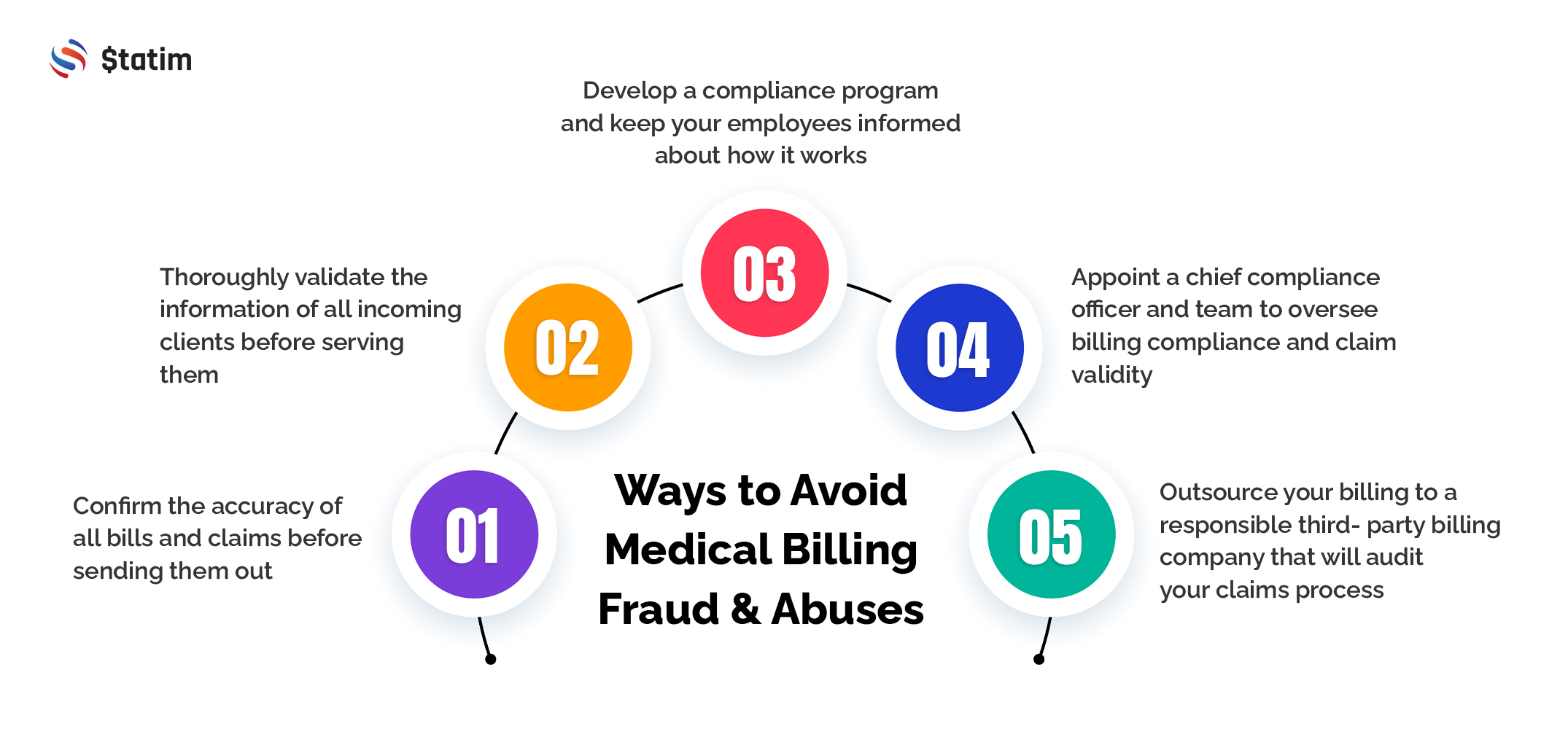
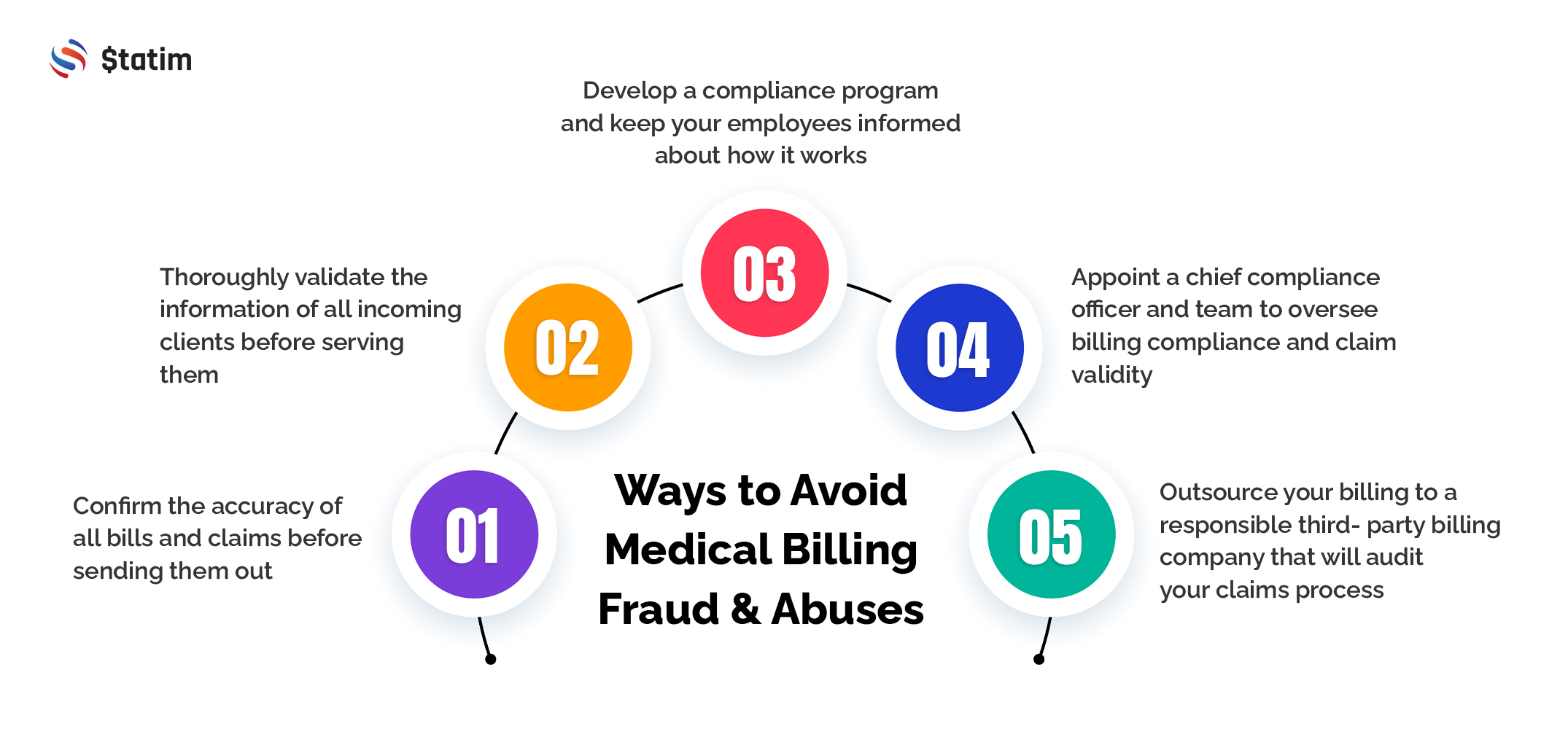
Medical billing fraud can be bad for both providers and clients and when it happens it usually means lost funds for both patients and insurance partners. Sometimes, it can pose legal risks to your practice and even endanger the health of your patients.
Fortunately, with a little bit of vigilance and pre-planning, you can prevent frauds and abuses from occurring and develop a system of action for when it does occur. Here are some steps you can take to avoid medical billing fraud and abuse.
- Thoroughly validate the information of all incoming clients before serving them
- Confirm the accuracy of all bills and claims before sending them out
- Develop a compliance program and keep your employees informed about how it works
- Appoint a chief compliance officer and team to oversee billing compliance and claim validity
- Outsource your billing to a responsible third-party billing company that will audit your claims process
Why Minimizing Medical Billing Errors is Essential for Your Medical Practice
Medical billing errors slow down the claims process, lowering the efficiency and total revenue of your medical practice day to day.
Coding errors that make it to the final billing statement can negatively impact patients who are up charged for services never received. These errors become more commonplace for higher bills where more services are rendered. Bills $10,000 or more, for example, can cost clients $1300 in billing errors.
On the provider’s side, errors in coding can also result in billing statements that are less than the rendered amount. This can lead to a loss of revenue for providers as well as their medical staff.
For a medical practice, coding and billing errors are a one-way ticket to claim rejection. When this happens, the bill is sent back to the provider to be reworked, costing additional time and resources. It is estimated that the average claim costs $118 to be appealed. It can also cause compliance issues at the state or federal level which may over time, result in fines, loss of accreditation, and loss of contracts or partnerships.
Improve Your Billing and Coding Accuracy with Statim LLC
Take the guesswork out of medical billing and coding with Statim LLC. We are a medical billing company located in Southern California. Our multi-stepped approach to medical billing reduces billing fraud, abuse, and errors while helping you save money. For more information on how we make medical billing easier call us at 888-544-3537.
Citations
FBI. (2016, June 1). Health Care Fraud. FBI. Retrieved October 22, 2021, from https://www.fbi.gov/scams-and-safety/common-scams-and-crimes/health-care-fraud.
Gooch, K. (n.d.). Denial rework costs providers roughly $118 per claim: 4 takeaways. Becker’s Hospital Review. Retrieved October 22, 2021, from https://www.beckershospitalreview.com/finance/denial-rework-costs-providers-roughly-118-per-claim-4-takeaways.html#:~:text=A%20vast%20majority%20(63%20percent,billion%20in%20administrative%20costs%20nationwide.
How providers can detect, prevent healthcare fraud and abuse. RevCycleIntelligence. (2021, June 21). Retrieved October 22, 2021, from https://revcycleintelligence.com/features/how-providers-can-detect-prevent-healthcare-fraud-and-abuse.
Varn, M. (2018, January 25). Why clients should care about medical billing errors. Employee Benefit News. Retrieved October 22, 2021, from https://www.benefitnews.com/advisers/opinion/why-clients-should-care-about-medical-billing-errors-and-what-they-should-do-about-it.
